Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Foot Wounds and the Importance of Off-Loading

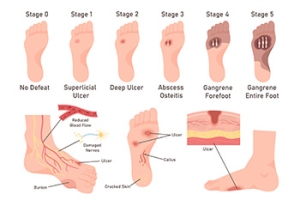
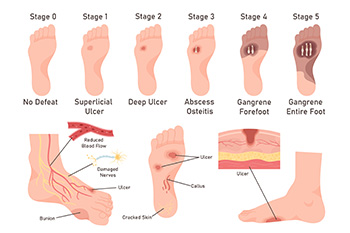
A wound of the foot is an open sore or injury that can result from trauma, pressure, poor circulation, or underlying medical conditions. These wounds can be slow to heal and may lead to serious complications, if not properly managed. Off-loading practices are essential for recovery as they relieve pressure from the affected area, allowing tissues to heal and reducing the risk of infection or further damage. Techniques include wearing specialized footwear, padding, casts, or orthotic devices. A podiatrist can evaluate the wound, create a personalized off-loading plan, and provide advanced treatments for faster healing. If you have a foot wound, it is strongly suggested that you promptly schedule an appointment with a podiatrist who can effectively treat this potentially serious condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Apple Podiatry Group. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please contact our offices located in Arlington Fort Worth, And Flower Mound, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
High Heels in Moderation
Wearing high heels regularly can take a toll on your body over time, and may produce weakened ligaments, lower back and knee pain, bunions, corns, calluses, plantar fasciitis, hammertoe, Morton’s neuroma, sesamoiditis, stiffened/shortened Achilles tendons, ankle sprains, and more. Women who are not dissuaded completely from wearing high heels can try to minimize their harmful effects with a few modifications. Shoes should be properly fitted and not too small. Foot size changes with age, childbirth, and fluctuations in weight, and feet should be measured for length and width with every shoe purchase. Heels should not be worn every day—only once in a while or on special occasions. Pencil-thin stilettos should be switched out with wider-heeled shoes which distribute body weight more evenly across the heel, or platforms or wedges that offer more stability and support. T-strap or Mary Jane styles help prevent the foot from sliding forward into the narrower part of the shoe, and also keep it more aligned evenly over the arch. A podiatrist may have additional footwear advice as well as the ability to create custom orthotics for support and to relieve pressure points on the foot caused by high heels.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact one of our podiatrists from Apple Podiatry Group. Our doctors can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions, please feel free to contact our offices located in Arlington Fort Worth, And Flower Mound, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Effect of High Heels on the Feet
High heels are uncomfortable, but many women sacrifice comfort to be stylish. There are many problems that stem from wearing high heels, however these issues can be avoided by wearing proper shoes.
Heels are bad because they push your weight forward toward the fall of the foot. The higher the heel is, the more weight and pressure get shifted. This process causes the back to hyperextend backwards to counterbalance which may cause pain in the leg, hip, and back. Consequently, major posture problems may occur, and these issues may eventually become permanent.
Wearing high heels is one of the leading cause of ingrown toenails. Heels create a great deal of pressure on the big toenails which disrupts proper toenail growth. This may eventually lead to the big toenail growing into the skin. Another common problem that stems from high heels is bunions. If bunions go untreated, they can cause serious scar tissue to form along with severe pain.
However, there are ways to minimize the harmful risks associated with wearing heels. You should try to massage and stretch your legs and feet after wearing heels for an extended time. Stretching helps prevent the Achilles tendons and calf muscles from becoming too tight. A good substitute for heels are platforms which provide a better surface area to evenly distribute the body’s weight.
If you are experiencing any painful foot conditions from wearing high heels, you should consult with your podiatrist right away.
Limb Salvage for Diabetic Patients With Foot Ulcers
Limb salvage refers to advanced medical treatments designed to prevent limb loss in patients with severe diabetic foot ulcers. These ulcers develop from poor circulation, nerve damage, and slow healing associated with diabetes. The goal of limb salvage is to remove infected or dead tissue, restore blood flow, and promote healing to preserve the affected limb. A podiatrist plays a vital role by managing wound care, controlling infection, and coordinating specialized treatments such as vascular therapy or offloading techniques. Early intervention greatly improves outcomes and helps patients maintain mobility and quality of life. For expert diabetic foot care and limb preservation, it is suggested that you are under the care of a podiatrist who can discuss the benefits of this type of surgery.
Diabetic Limb Salvage
Diabetic limb salvage can be an effective way in preventing the need for limb amputation. If you have a foot ulcer and diabetes, consult with one of our podiatrists from Apple Podiatry Group. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Diabetic Limb Salvage?
Diabetic limb salvage is the attempt of saving a limb, such as the foot, that has an infected ulcer, from amputation. Podiatrists also try to make sure that there is enough function in the foot after the salvage that it is still usable. Those with diabetes experience poor blood circulation, which prevents proper healing of an ulcer. If the ulcer is left uncheck, it could become infected, which could result in the need for amputation.
Diabetes is the number one cause of non-traumatic amputations in the United States. Amputation has been found to lead to higher mortality rates. This translates into higher healthcare costs, and a reduced quality of life and mobility for amputees. Podiatrists have attempted to increase the prevalence of limb salvage in an attempt to solve these issues.
Diagnosis and Treatment
Limb salvage teams have grown in recent years that utilize a number of different treatments to save the infected limb. This includes podiatrists that specialize in wound care, rehabilitation, orthotics, and surgery. Through a combination of these methods, limb salvage has been found to be an effective treatment for infected limbs, and as an alternative to amputation. Podiatrists will first evaluate the potential for limb salvage and determine if the limb can be saved or must be amputated.
If you have any questions, please feel free to contact our offices located in Arlington Fort Worth, And Flower Mound, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetic Limb Salvage
Limb salvage is a procedure that involves saving a lower extremity from amputation. In podiatry, limb amputation often occurs as a result of diabetes. The fundamental goal of limb salvage is to restore and maintain stability and movement of the affected lower extremity.
The procedure typically involves removing the diseased tissue and a small portion of the surrounding healthy tissue, as well as the removal of any affected bone if necessary. If bone is removed it is then replaced with prostheses, or synthetic metal rods or plates, or grafts from either the patient’s body or a donor. Limb salvage is typically the preferred choice of procedure over amputation, as the procedure preserves both the patient’s appearance and allows for the greatest possible degree of function in the affected limb.
Upon diagnosis and determining that limb salvage is the appropriate treatment, the podiatrist may enlist the help of a physical and/or occupational therapist to prepare the patient for surgery by introducing various muscle-strengthening, walking, and range of motion exercises. Such exercises may be continued as rehabilitation post-procedure.
Causes of Foot and Ankle Injuries in Skaters

Skating is a beloved activity for many, but foot and ankle injuries can hinder both enjoyment and performance. Improperly fitted skates often lead to corns, calluses, bunions, and bunionettes, causing discomfort and negatively affecting skating ability. Additionally, ankle pain and weakness are prevalent among skaters, making them susceptible to sprains and overuse injuries like Achilles tendonitis. Skaters with biomechanical imbalances, such as flat feet or high arches, are at further risk of developing plantar fasciitis and heel pain. One way to avoid these issues involves wearing properly fitting footwear and attentive foot care. Investing in well-fitted skates and footwear tailored to individual foot needs is essential. Plus, seeking prompt treatment for persistent foot pain from a podiatrist ensures optimal skating performance and long-term foot health. By taking proactive measures to prevent injury, skaters can continue enjoying their favorite activity without discomfort or limitations. If you have skating-related foot or ankle pain, it is suggested that you schedule an appointment with a podiatrist.
Ankle and foot injuries are common among athletes and in many sports. They can be caused by several problems and may be potentially serious. If you are feeling pain or think you were injured in a sporting event or when exercising, consult with one of our podiatrists from Apple Podiatry Group. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Common Injuries
The most common injuries that occur in sporting activities include:
- Achilles Tendonitis
- Achilles Tendon Rupture
- Ankle Sprains
- Broken Foot
- Plantar Fasciitis
- Stress Fractures
- Turf Toe
Symptoms
Symptoms vary depending upon the injury and in some cases, there may be no symptoms at all. However, in most cases, some form of symptom is experienced. Pain, aching, burning, bruising, tenderness, tightness or stiffness, sensation loss, difficulty moving, and swelling are the most common symptoms.
Treatment
Just as symptoms vary depending upon the injury, so do treatment options. A common treatment method is known as the RICE method. This method involves rest, applying ice, compression and elevating the afflicted foot or ankle. If the injury appears to be more serious, surgery might be required, such as arthroscopic or reconstructive surgery. Lastly, rehabilitation or therapy might be needed to gain full functionality in the afflicted area. Any discomfort experienced by an athlete must be evaluated by a licensed, reputable medical professional.
If you have any questions please contact our offices located in Arlington Fort Worth, And Flower Mound, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are common among athletes and those who exercise frequently. Most of these injuries are non-life-threatening and can heal in weeks with proper treatment and care. Serious injuries, however, require urgent medical treatment.
Common minor injuries include ankle sprains, ankle strains, Achilles tendonitis, plantar fasciitis, stress fractures, and turf toe. An ankle sprain is when the ligaments in the ankle have either become stretched or torn. When the muscle or tendon is stretched or torn, it is an ankle strain. When the big toe is sprained, it is known as turf toe. Achilles tendonitis is the overuse and inflammation of the Achilles tendon. Plantar fasciitis is the inflammation of the plantar fascia and generally occurs from overuse in athletics. Stress fractures are also caused from overuse and are small cracks in the bone.
Achilles tendon ruptures are common, but more serious. This injury occurs when the Achilles tendon, the largest tendon in the body, ruptures. In most cases, this causes severe pain and difficulty walking; some who have experienced this injury have reported, however, no signs or symptoms. A laceration is a deep cut that can occur anywhere on the body. Lacerations on the foot are rarer, but can occur from things like metal cleats landing on the foot.
Treatment options cover a wide range of methods based upon the injury and its severity. Conditions like plantar fasciitis, stress fractures, Achilles tendonitis, turf toe and ankle sprains/ strains can heal on their own without immediate medical care, but seeing a podiatrist to monitor the injury is always recommended. Following the RICE (Rest, Icing, Compression, and Elevation) protocol is generally enough to treat minor injuries. This means resting the foot by either keeping pressure off the foot or not walking at all. Icing the injury will help reduce swelling and pain. Compressing the wound with a wrap will immobilize and help promote healing. Finally, keeping the wound elevated will also reduce swelling and also help the healing process.
It is important to note that even minor injuries can vary in severity, with grade one being a minor injury and grade three requiring urgent care by a podiatrist. Achilles tendon ruptures and lacerations on the foot generally require urgent medical care and treatment options that need a podiatrist. These could include imaging tests, stitches for cuts, rehabilitation, and casts or braces. Every case is different, however, so it is always recommended to see a podiatrist when pain in the foot does not disappear.